During the wait for my MDP (Multi disciplinary panel) I took full advantage of any sympathy food to come my way. You would be surprised by how far getting knocked off an e-scooter gets you in terms of free-food! On the run up to Christmas 2022 I honestly had one of the most jam packed social calendars of my life with everyone wanting to hear the full gory details of my accident and of course show their love and support. Here are a few shots of me enjoying said socials!


There was still the small issue of my brain tumor who I had subsequently decided to name Bob, from a series of books entitled ‘The Bobiverse’ by Dennis E. Taylor. You must check them out if you get the chance. For now I was keeping my cards close to my chest until I knew more of what I was dealing with.
One week went by with no word about my upcoming MDP. I was walking quite happily by this stage, sticking to comfortable footwear wherever possible and by the second week it was time to have my toe sutures removed by the practice nurse. She actually had a trainee nurse in with her who hadn’t removed sutures before. I’m all for learning & developing clinical skills via practical experiences so I let her practice on me. She completed the task very well, with only the slightest of guidance from the practice nurse & was grateful for the opportunity to learn.
By the start of the second week my hopes began to diminish about whether or not the MDP would happen this side of Christmas. I began to try to chase up the various secretary’s of the several Neuro-Oncologists in Southmead hospital to see if there had been any news. Suddenly I received a call back while out walking in Bristol’s harborside. It was Thursday 22nd of December and the secretary on the phone asked if I was able to attend a clinic on the Friday 23rd. Of course, this was what I had been hoping for and I quickly re-arranged my flight home for the following day, Christmas eve.
One of my weak points is that I don’t like asking for help, I was even reluctant to bring anyone to my appointment initially. However, I accepted the invitation to have a tarot card reading by a friend called Zara who I consider to be a little gifted in these sort of things. Now, full disclaimer, I don’t how much to read into the tarot but what is curious is that I received the 7 of swords card in a blockage position as my present card. Basically, this was the universe’s way of telling me that my lone wolf attitude was holding me back and I would be more free without it and to let others’ in. Which was exactly what I needed to hear at the time.
I decided later that evening to bring along Gerard to my appointment. Gerard is one of the company’s directors. A fellow colleague & mentor to name a few of the more official titles’ I could give him. Mostly, I trusted him with being able to process the facts of the situation, anticipate the likely consequences and to gauge the time spent out of work in recovery mode. It hadn’t seemed like long at all since we had enjoyed making a nuisance of ourselves at the work’s Christmas party. Little did I know he’d be accompanying me to an appointment such as this not four weeks later. But, I was grateful he did. Firstly for the moral support and secondly as a spare pair of ears as I knew from my own experience that patients are able to recall only 30% of what’s mentioned in the room and I was unsure if I’d prove to be any better!

Gerard revealed he had some previous knowledge about the consultant I was scheduled to see for my appointment. ‘Dr. Venkat Iyer’ was his name to which he added that I was seeing ‘The Boss’ and that I was good hands. This gave me reassurance.
The appointment was at Southmead hospital and as hospitals go it was an architectural masterpiece. Somehow managing to perform all the necessities of a functional hospital while combined with having high vaulted ceilings which created the illusion of having vast amounts of cavernous space overhead. Yet it did not lose the ability to provide human touches where necessary, like having a multi-faith prayer room, modern artwork for decoration and the presence of a piano that could be played by anyone who had the skill/inclination.
‘Gates’ very much like you would see in an airport lined the walls. Although, instead of transporting you to some tropical destination or another, these ones usually resulted in you receiving a life changing diagnosis. Gate 36 was for Neuro-oncology where I awaited such information. We had a short wait while Gerard and I discussed how the eye hospital could learn a thing or two from this particular setup. We were then called in and introduced to the meet team who would be looking after me.
They included, Dr. Venkat Iyer & his registrar Dr. Raenette David. A support worker called Gary along with representatives from both the Occupational therapy and speech and language teams.
After inviting us to have a seat with the seven of us sat in a rough circle, Dr. Iyer recognized Gerard immediately, with that he quipped that Gerard used to have more hair last time they met! Which was even funnier with the reality that Dr Iyer is completely bald himself! That one phrase broke right through the ice and put everyone in the room at ease and I was thankful for that!
I was then asked by Dr. Iyer to explain the situation as it stood to the best of my understanding. This felt like a slight test aimed not only gauge my current level of understanding, but also how much I had been told at the BRI and moreover how I was dealing this information.
I re-told my story of being involved in a road traffic accident after leaving work. This had appeared to bring on a seizure and upon further testing via CT and MRI scans it was suspected that I had low grade glioma. Later receiving an all-clear result from the subsequent chest and abdominal CT scans.
Dr Iyer seemed satisfied by the synopsis I had given and went on to describe what they suggested doing about my current situation. It was strongly recommended that I undergo a procedure known as an ‘awake craniotomy’. Any procedure starting with the word ‘awake’ was never good, I thought to myself!
Dr Iyer spoke with professionalism and a calming, precise nature that inspired confidence. He went on to explain that the rationale behind doing it this way i.e. never completely the knocking the patient out with a general anesthetic, allowed for additional testing and monitoring to be completed in situ, giving a more precise outcome. The aim was to take as much as possible out while still persevering normal brain function (Whether or not I am completely normal its still up for debate.)
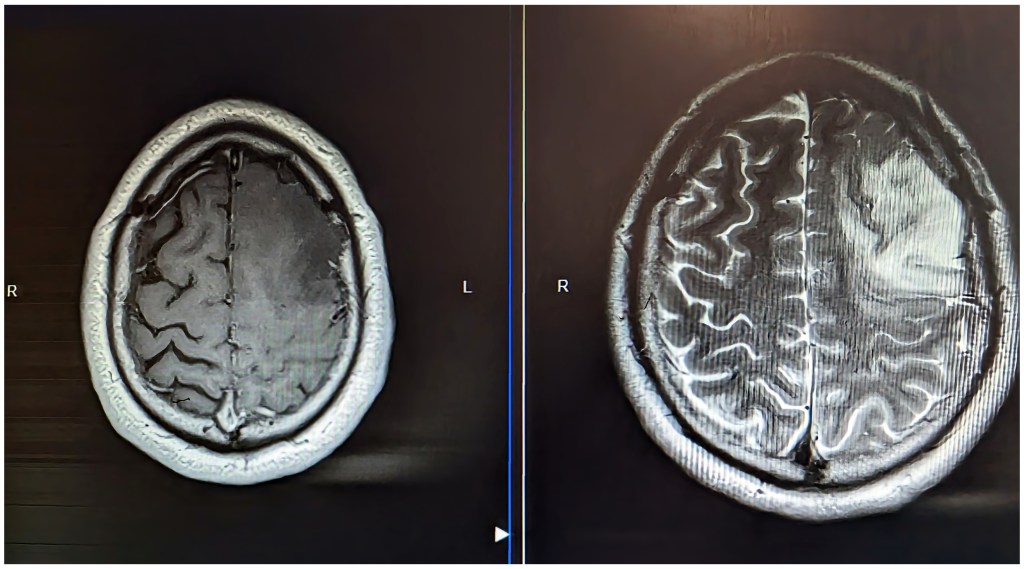
He then took the opportunity to show me the true extent of my tumor from the MRI and was clearly well versed interpreting the scans and assessing the likely impacts on the underlying structures. The tumor showed up as the white mass on my left frontal lobe (Far right hand side of this image) Again, what struck me about this image it’s the sheer size and that I had been completely asymptomatic prior to the accident.
So doing it while I was awake was basically the only the option which would allow for a greater degree of accuracy and more acceptable margins for error during the removal which would was estimated to take 6-7 hours it all said and done.
Dr Iyer went on to explain in his calm tone, that there were certain unavoidable risks to this surgery and that no procedure was without risk. He estimated the risk of serious complications to be less that 10%. With a less than 1% chance of loss of life. Included in the list of what were considered to be the most serious complications, was the risk of complete hemiplegia (Paralysis of the right hand side) Loss of function or fluency with speech, COVID-19 and the potential for leakage of CSF (Cerebral spinal fluid.)
It was at this stage he used the analogy of it being a bit like removing ink from water. That it was both a tricky and time consuming job especially when working out which areas were tumor and which were normal brain tissue. He mentioned that one of the ways which was commonly used to identify the difference was to play little word games on a laptop during the surgery. This would allow the for stimulation of certain areas of the brain and in doing so revealing their importance to functions like speech & language.
So hearing all of this I was confident I had come to a decision. I had already read a bit about it on the run up to this appointment and was aware that the awake craniotomy was the most likely procedure to be suggested in my clinical situation. Moreover, the way I looked things, I had been given an opportunity to act now and that a timely resection was the best way achieve a positive clinical outcome and was linked to increased long term survival and prognosis.
I understood that was there was the potential to need adjunctive therapies afterward i.e. radiotherapy or chemotherapy depending on how satisfied they were after the initial surgery but time would tell on that front and parts of ‘Bob’ would likely be sent for further analysis and testing to work out what he was exactly.
It was an interesting thought exercise to consider the psychology of risk. For example, if I had a one in ten chance of winning the lottery, I would feel would like I was in for a decent shot! But turned on its head the chances were slightly less appealing when accepting a 10% risk of a surgical complication, the thought was slightly sobering. Nonetheless I’d considered the risks to acceptably low given that ‘Bob’ was only going to get bigger and eventually cause me trouble and by that stage would likely be a higher grade of tumor. My mind had been made up. Bob’s days were numbered!
Also I was confident that, given enough time I could adapt to any unforeseen complication, be what may. Such is life and sometimes there are advantages in having limited options. Beside’s I was more than willing place my trust in my surgical team who had been very impressive thus far. I was all set to roll the dice of life and hope for the best.
With the decision made there was some consent paperwork to fill in. An OT named Charlie began some ‘pre-habilitation’ work. Essentially a newish scheme introduced to help assess the pre-surgical need of patients so that the transition post surgery could be made as smoothly as possible. Dr Iyer had some holiday scheduled for the majority of January. As we didn’t think ‘Bob’ was going anywhere quickly we set a target date for my Op to be scheduled for early February and I wished him to have a restful and pleasant holiday.
Gerard and I left feeling very positive about overall experience and the professionalism from the Neuro-oncology team which was high praise coming from picky so and so’s like ourselves. I thanked Gerard for coming along for the ride too, I was grateful to have had him there by my side.
So there I was, two days before Christmas with an awful lot to think about, but with arguably the most perspective and clarity than I ever had in life thus far. The next few months were going to be an interesting ride for sure. I was suddenly reminded of the quote:
“A man lives two lives. The second begins when he realises he has just one.”
Stay tuned for the next blog as this covers the lead up to surgery and my January of two halves. Work hard. Play harder.

“Thanks so much for everyone thats been there for me since my diagnosis. If you’ve sent me a text that’s made me smile that will have been enough .”
— Connor
JustGiving
Some of my good friends have set up a JustGiving page for me. It’s truly an honor and a privilege to have such thoughtful and generous people in my life.
If you’d like to donate to it here’s the link.

About my Story
I am committed to bringing you my true, raw and unfiltered experiences living with a brain tumour. Expect a humorous take on a gritty and often difficult subject. Through the lens of positivity, I examine the daily struggles and challenges of those of us living with brain tumours.
I aim to advocate, educate and shed light on an often misunderstood subject.
Newsletter
Subscribe now to Keep up to date with my blog and all the happenings in the world of brain tumours.
Leave a reply to Shamirra Javed Cancel reply