Chapter 13
Navigating Scanxiety: Insights on Tumor Progression
Time seemed to fly by. Before we knew it, it was Christmas 2024. I was working through most of the Christmas and New Year’s period this year, so the days passed quickly.

Jessie and I spent it together in Bristol, a lovely first for both of us. We had a rather ‘unconventional’ Indian takeaway on Christmas Eve, watched old Christmas films, and enjoyed some much-needed ‘us’ time. By early January 2025, it was already time for another MRI.

By this stage, I like to make my appointments efficient but enjoyable with a little reward at the end. I usually cycle through Bristol city centre to Southmead hospital (4.5 km), then get the scan done, and follow that up with a nice coffee on the way home.

It turns an appointment that might otherwise feel like a chore into something I can look forward to,
By shifting the: “I have to” to “I get to.”
This is a powerful mindset shift circulating on social media right now.
I believe Dwayne “The Rock” Johnson has taken some credit for this, but the original message actually comes from the motivational speaker Inky Johnson. His story is incredibly moving, and his delivery is full of passion. I’ll post the video link below so you can check it out when when you are having a low day, he’ll snap you out of it.
As I write this, I am thinking of creating a ‘Toolbox.’
I think this is a great name for a page dedicated to all the tricks and techniques I’ve found helpful as someone who deals with heavy things from time to time, in the hopes that it can be of use to someone else. That way,
- I can come back to them again, all organised in one place
- People can read and select the ones that resonate with them.
So I’ll add a link here when the ‘Toolbox’ page is up and running. Feel free to take a look. I’ll also put a link on my site’s main page.
Anyways, back to story, on this particular scan, I wouldn’t receive the results for another seven long weeks.

I think the hardest part of these moments is the waiting, the time that passes between the scan and the silence. Not knowing. Not hearing anything. Life continues around you, with its moments of joy, sadness, frustration… but through it all, there’s a dark shadow trailing you just out of sight. Only you can see it.
To use an Optometry metaphor, It’s like a floater! One of those irritating things that dances in your peripheral vision. You can’t quite focus on it, and every time you try, it shifts away. But it’s often there lurking away.

To be honest, I sometimes forget I have a brain tumour. I get lost in a good day, a happy moment or a really intense period at work, and then it hits me again.
‘Oh right… Sh*t…I’m still waiting on my scan results’
I enjoy the moments I forget, but the melancholy I feel when I remember the truth is rarely worth it.
I have now accepted that even the happiest moments have to be experienced with the knowledge that the rug could be quietly pulled out from under you without warning.
Making peace with this uncertainty is what I’ve learned to do. I’m still not 100% comfortable with it, but I’m getting there.

It’s a heavy weight to bear at times, but then I remind myself that many others are facing far tougher battles, some lying in hospital beds, dreaming of the chances I still have.
The chance to live, to move, to be well enough to explore and experience the world. That perspective helps quiet the negative thoughts and brings me back to living.

Scanxiety
Finally, the MDP results came back. It was late February, and I was fighting off waves of what’s known as “scanxiety” in the brain tumour community. It’s fairly typical for results to take this long; the Multidisciplinary Panel (MDP) needed time to assess the tumour’s status and decide on the best course of action.
I kept telling myself that this was a good thing. That worrying was pointless; I’d soon be in a position of clarity, and when the time came, I’d deal with it. Rationally. Calmly.
The fact that I also had a telephone appointment booked for me also boded well. Surely, if they had bad news to deliver, they would do it in person. Right?

Wrong. The results revealed something I had quietly dreaded.
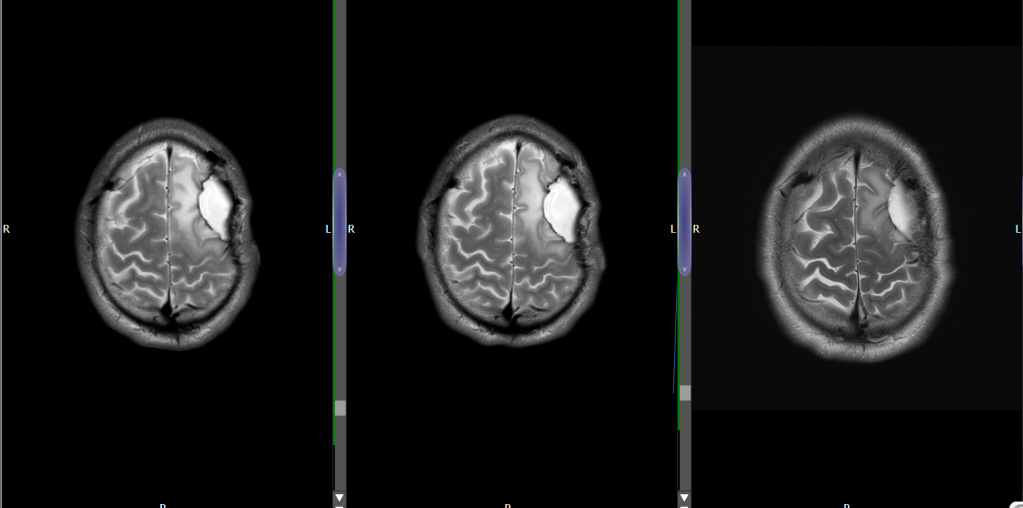
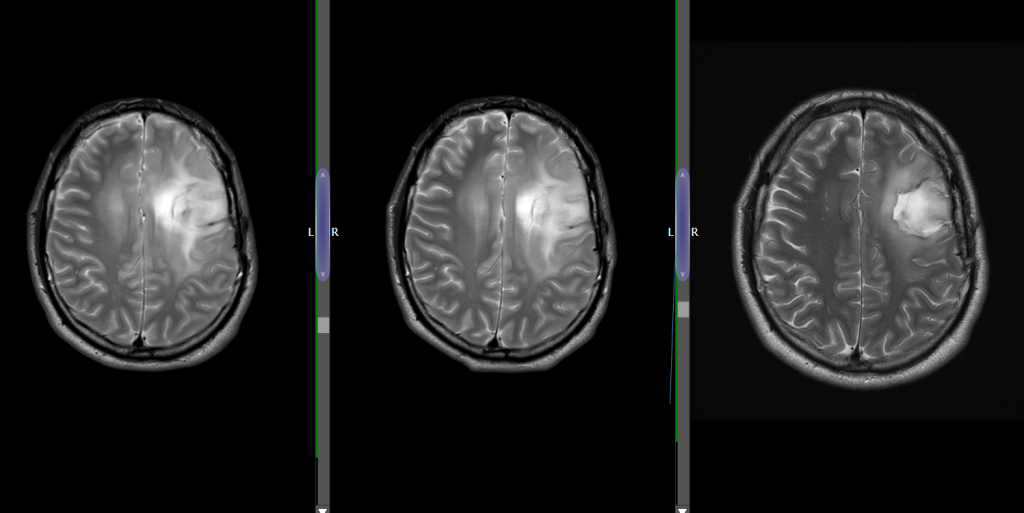
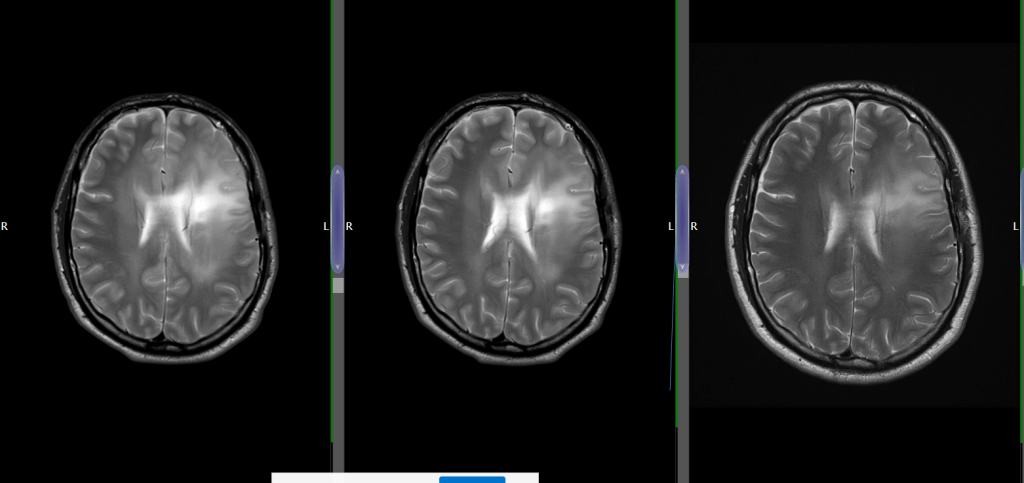
My tumour, or what was left of it, was lighting up more brightly and absorbing more contrast dye than before. That could only mean one thing: Progression.
There was no clear suggestion or evidence that it had transformed into a Grade III or IV, but the scan showed definite areas of increased activity compared to 2023 and 2024. I could see it for myself. And then came my consultant’s words:
“Your tumour has progressed.”
Words I’d hoped not to hear for a long time. I had been hoping for the best, preparing for the worst, but it still hit hard.
Progression
Jess was distraught. The news rippled through every part of our lives, uncertainty, fear, and difficult decisions all over again.
To make things sting a little more, the call that came to deliver all this news came over an hour late, and likely wouldn’t have happened at all if I hadn’t prompted it.

The scheduled appointment time came and went. I could feel the knot of nervous anticipation tightening in my stomach. Fifteen minutes passed. ‘Cool, cool I thought, the clinic’s probably running a little late, it’s happened me before’ Then thirty minutes passed. The knot doubled. Then forty-five. ‘Any time now!?’ I’m pretty chilled about clinics running late, but this was getting ridiculous. Eventually, I said enough is enough and I took action. I looked up the out-of-hours number and called. A helpful on-call neurosurgeon picked up and agreed to look into this for me.
The on-call surgeon likely nudged my consultant. I like to imagine the message was delivered via WhatsApp, reminding him I’d been forgotten, and my consultant face-palming and muttering several expletives. 😂
It can’t be easy managing such an intense caseload, especially with such heavy subject matter constantly immersed in that environment and often having to deliver bad news. That kind of work can really wear a person down. That said, when it comes to brain tumours and telephone consultations, it might be worth insisting for an in-person appointments in future. 😐
My consultant finally called 90 minutes late, delivering the news in a direct and fairly matter-of-fact manner, with barely a word of apology for the delay.
But by that point, I was focused entirely on one word: “Progression.”
This wasn’t the worst-case scenario: That would have been hearing that the tumour had advanced to a Grade III or IV, or that it was now inoperable.
Nevertheless, it was still a serious blow, not the news I was hoping for, and delivered in a way that stung all the more, the delivery lacking in compassion, empathy, and to add insult to injury, much later than anticipated.
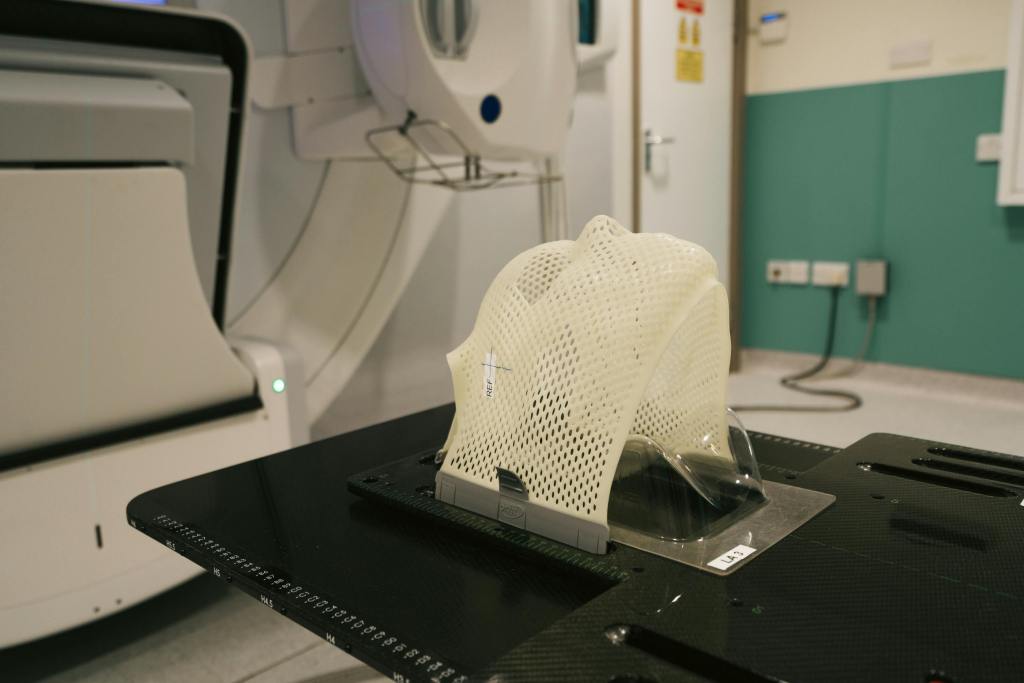
I felt let down, with my trust in the clinician shaken. Scheduling mistakes happen and I resolved to in that moment, concentrate on what was important and what we could do about it. See Below my actual brain scans. Note the lighter areas lighting up on the more recent scans.
Together, we reviewed the MDP report, and the recommendation was that I reconsider radiotherapy and chemotherapy. My Consultant cautiously agreed to look once more into accessing the drug Vorasidenib, which I had been doggedly pursuing for some time, and I was already in a battle to access it myself. He agreed to refer me to another treatment centre in an attempt to seek access, but I could tell from his tone that he didn’t think it was likely or worth my time.
The Fight for Vorasidenib
You may remember I was closely following the progress of a new drug called Vorasidenib. After it passed its Phase III INDIGO trial, I began doing everything I could to access it.
Vorasidenib is a targeted therapy for IDH1- or IDH2-mutant low-grade gliomas (My type of tumour.) It has been shown to double progression-free survival and reduce seizure activity. While not free from side effects the potential benefits are significant, particularly before radiotherapy or chemotherapy.

The catch is: if you’ve already had radiotherapy and chemotherapy, there’s no reliable evidence that Vorasidenib works effectively. So, to access the drug currently, it must be administered before those treatments take place.
After FDA approval in the U.S. I hoped the UK would move quickly. But without MHRA licensing and NICE approval, expected late 2025 it isn’t routinely available on the NHS. In the meantime, some Oncology centres offer it through Servier’s compassionate access programme, creating a postcode lottery. Sadly bristol isn’t one of them.
I therefore tried every other route I knew of to attain it:
Unfortunately Using my Private healthcare insurance was a no-go, as it’s unlicensed in the UK.

I also tried connecting Servier directly with my oncology team June 2024. It looked positive in the beginning. They exchanged emails, a dialogue began, they held talks in an attempt to get something set up. I was later told that they ran into red tape and the process stalled.
By January 2025, my scans showed tumour progression, making me a less favourable candidate.
A final ‘hail mary’ effort to attain access came in the form of a referral to a participating centre in Birmingham: I went through the formal approval process and, for a while, there was a glimmer of hope. But after further review via MDP and with progression already detected doubts grew over whether Vorasidenib would help me now. It felt like shutting the stable door after the horse had bolted.

The recommendation was to move to standard treatment.
Still, when I think about it even today, I find myself frustrated and emotional, that if the compassionate access scheme had been more widely available across NHS trusts, I might have qualified for the drug sooner. The first UK patients started receiving it in summer 2024, and still feels unfortunate to me that I wasn’t one of them.
Vorasidenib isn’t a miracle cure, but it represents a rare glimmer of hope, the first step toward a new generation of treatments, while the system still leans on decades-old therapies that have been extensively researched, tried and tested but come with significant risk of adverse reactions and long term side affects’.
For now one door has closed, but not locked. I’ll keep it in my sights, ready for when the evidence and access align.

All roads lead to Radiotherapy:
By mid-April, my decisions all pointed to one direction. The road to get there had been anything but simple. There had been weeks of consultations, second opinions, and in-depth discussions with specialists in oncology and neurology.
Each appointment added a new layer of insight yet complexity, a fresh variable to weigh up. Jessie and I did our own deep dive into the research, too, which was mentally and emotionally exhausting, especially while trying to keep life ticking over with work and a sense of normality. Eventually, the pieces began to align, and a clearer timeline came into view.

With the decision made to pursue a 6 week course of radiotherapy then followed by PCV Chemotherapy.
Jessie and I began mapping out the months ahead. We took advantage of when our first radio session could was to scheduled for. First, a short break in the Canary Islands to reset and recharge. Then, a special time in May when our families would come together.
A moment to steady ourselves before the next chapter: six weeks of radiotherapy through June and July, followed by chemotherapy starting in August and stretching into the months beyond.

With our plan set and our resolve strengthened, we were ready to face whatever came next. The ACDC’s classic track suddenly comes mind.
“For those about to Rock, we salute you.”

“Thanks so much for everyone thats been there for me since my diagnosis. If you’ve sent me a text that’s made me smile that will have been enough .”
— Connor
JustGiving
Some of my good friends have set up a JustGiving page for me. It’s truly an honor and a privilege to have such thoughtful and generous people in my life.
If you’d like to donate to it here’s the link.

About my Story
I am committed to bringing you my true, raw and unfiltered experiences living with a brain tumour. Expect a humorous take on a gritty and often difficult subject. Through the lens of positivity, I examine the daily struggles and challenges of those of us living with brain tumours.
I aim to advocate, educate and shed light on an often misunderstood subject.
Newsletter
Subscribe now to Keep up to date with my blog and all the happenings in the world of brain tumours.
Leave a comment